Acupuncture outperforms routine drug therapy for the treatment of pain due to indigestion. In a randomized clinical trial, acupuncture produced superior patient outcomes over patients using domperidone for the treatment of functional dyspepsia (non-ulcer stomach pain, often with distention, nausea, or belching). In addition, patients receiving acupuncture had a greater improvement in sleep duration and quality over functional dyspepsia patients taking drug therapy.
Domperidone is a dopamine antagonist used to treat gastrointestinal disorders, including gastroesophageal reflux disease (GERD), gastroparesis, nausea, and vomiting. As a gastroprokinetic agent, domperidone supports food transit by stimulating peristalsis. The results of the study indicate that acupuncture has a significantly more effective action on the promotion of digestion than domperidone.
Several indices indicate that acupuncture is a stronger treatment modality than domperidone for the treatment of functional dyspepsia. PSQI (Pittsburgh Sleep Quality Assessment) and SF-36 scores were better in the acupuncture study group. The SF-36 is a survey measuring overall patient health, including pain levels, functionality, and vitality. In addition, neuropeptide, motilin (a hormone that stimulates gastric activity), IL-1, IL-6, and TNF levels all indicate that acupuncture is a superior treatment modality. In summary, both objective and subjective findings indicate that acupuncture is safe and effective for the treatment of functional dyspepsia while yielding superior patient outcomes over routine drug therapy.
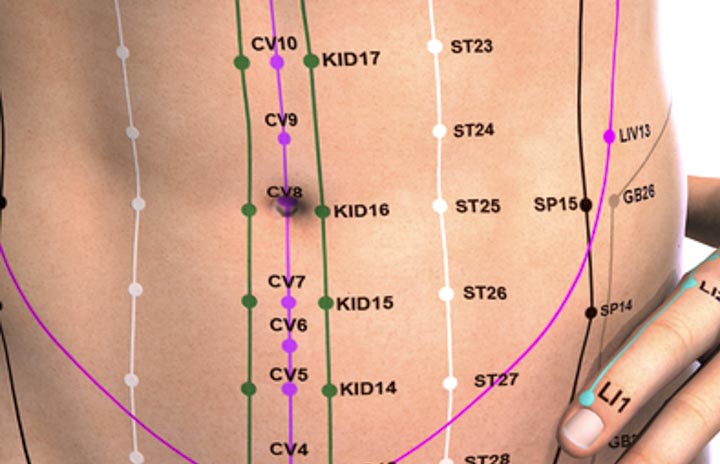
All patients were admitted to the study at the Yichang Central People’s Hospital of Three Gorges Dam from May 2013 to May 2015 and were randomly divided into 2 groups (acupuncture and drug). Patients receiving domperidone took 10 mg, 15 minutes prior to meals, three times per day. Patients receiving acupuncture were needled with identical acupoints:
ST36 (Zusanli)
PC6 (Neiguan)
ST25 (Tianshu)
Perpendicular insertion was applied to all points. Stimulation of deqi with mild reinforcing and reducing methods was employed. Needle retention time was 30 minutes per acupuncture session. Simultaneous application of moxibustion at ST36 was applied. One course of care consisted of 6 days of acupuncture therapy and two courses of care were applied.
Acupuncture and drug therapy both produced significant positive patient outcomes. However, acupuncture outperformed drug therapy. Wu et al. had similar findings, published in research entitled Analysis of therapeutic effect of acupuncture and moxibustion on functional dyspepsia. The total effective rate for acupuncture, based upon all data, was 95.4%. Drug therapy produced an 84.1% total effective rate.
References
Zeng LF, Tuo L. (2017). Effect of Acupuncture on Dyspepsia with Sleep Disorders. Liaoning Journal of Traditional Chinese Medicine. 2017,44(2): 359-361.
Wu ZL. (2017). Analysis of therapeutic effect of acupuncture and moxibustion on functional dyspepsia. Asia-Pacific Traditional Medicine. 2017,13(2): 112-113.
Ford AC, Bercik P, Morgan DG, et al. (2014). The Rome Ⅲ criteria for the diagnosis of functional dyspepsia in secondary care are not superior to previous definitions. Gastroenterology. 2014,146(4): 932-940.
Milini N, Filipovic B, Luki T, et al. (2014). Ultrasonography anlysis of gallbladder motility in patients with functional dyspepsia. European journal of internal medicine. 2014,25(2): 156-159.
Li X, Cao Y, Wong RKM, et al. (2013). Visceral and somatic sensory function in functional dyspepsia. Neurogastroenterology and motility. 2013, 25(3): 246-253.

![Diseases, Symptoms, tcm, [tcmwindow.com]](/uploadFile/adImg/2015/11/11/f5cbfcc0-4df5-4646-9b9a-f316651a0199.jpg)





