Electroacupuncture combined with Chinese herbal medicine navel paste outperforms drugs for alleviating post-stroke constipation. In a controlled investigation, acupuncture plus topical herbal medicine had a higher total effective rate and a higher complete recovery rate than drug therapy. In addition, acupuncture plus topical herbal medicine had a significantly lower failure rate than drug therapy.
Researchers (Xiong et al.) compared the therapeutic effects of electroacupuncture plus Chinese herbal medicine navel paste with that of a pharmaceutical medication. Two groups were compared. A Traditional Chinese Medicine (TCM) group received electroacupuncture to benefit circulation in the blood vessels and nerves. In addition, a Chinese herbal medicine navel paste was applied topically to the umbilicus region. The drug group received phenolphthalein, a diphenylmethane stimulant laxative, in tablet form. Phenolphthalein tablets are prescribed to relieve constipation. The TCM group achieved a 92.5% total treatment effective rate. The drug group achieved a 78.8% total effective rate.
The use of the Chinese herbal medicine navel paste in a TCM treatment protocol has deep historical roots. The 52 Bing Fang (Prescriptions for Fifty-two Diseases), a textbook written during the the Warring States Period (475–221 BCE), documents the treatment protocol and terms it Qizhi (Umbilicus Treatment). The researchers note that umbilicus treatment is "convenient, safe, and has a low adverse effect rate." Let’s take a look at how this treatment method is combined with modern electroacupuncture for the purposes of alleviating post-stroke constipation.
The study design was as follows. A total of 160 patients were randomly distributed into a control group and a treatment group, each consisting of 80 cases. The control group received drug therapy. The treatment group received acupuncture plus Chinese herbal medicine navel paste. All patients were diagnosed with post-stroke constipation between April 2013 and December 2015.
The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 50 males and 30 females. The average age in the treatment group was 60 (±5) years. The shortest course of disease was 15 days and the longest was 20 months. The control group was comprised of 52 males and 28 females. The average age in the control group was 60 (±5) years. The shortest course of disease was 18 days and the longest was 21 months. There were no significant statistical differences in terms of age, gender, and course of disease relevant to patient outcome measures.
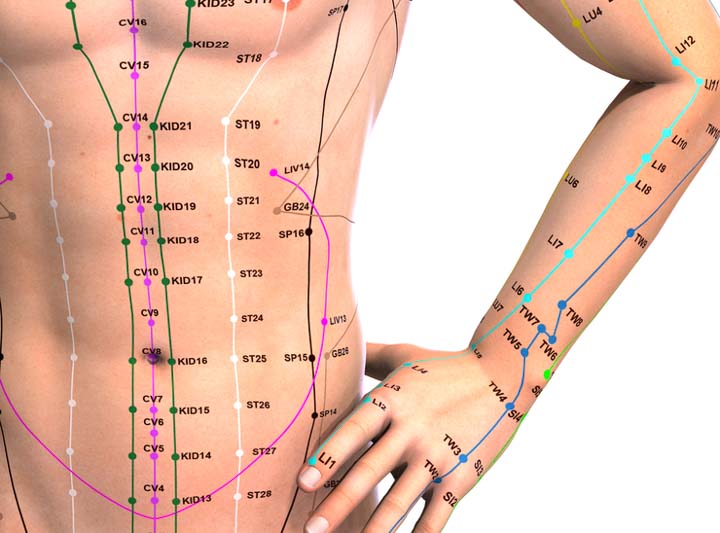
The drug group received 200 mg of oral phenolphthalein tablets, once per day, for 10 consecutive days. The Traditional Chinese Medicine group received electroacupuncture and the Chinese herbal medicine navel paste. The acupoints used for electroacupuncture treatment were the following:
ST25 (Tianshu)
SP14 (Fujie)
SP15 (Daheng)
ST29 (Guilai)
CV6 (Qihai)
CV4 (Guanyuan)
Qizhongsibian (Extra)
Jingzhong (Extra)
Manual acupuncture was applied prior to the administration of electroacupuncture. Upon disinfection of the acupoint sites, a 0.30 mm x 40 mm filiform acupuncture needle was inserted into the acupoints to a depth of 6–10 mm and manipulated with mild reinforcing and attenuating (Ping Bu Ping Xie) techniques. After elicitation of a deqi sensation, the acupuncture needles were connected to an electroacupuncture device. A disperse-dense wave was applied with an intensity level set to patient tolerance levels or until muscle contractions were observable. The needles were retained for 30 minutes, once electroacupuncture began. One 30 minute electroacupuncture session was conducted daily, for a total of 10 consecutive days. A navel Chinese herbal medicine was also applied, which contained the following herbs:
Da Huang 10 g
Mang Xiao 10 g
Hou Po 6 g
Zhi Shi 6 g
Huo Ma Ren 6 g
Yu Li Ren 6 g
Bing Pian 3 g
The aforementioned ingredients were ground into a powder and mixed with honey to produce a paste. A total of 3–5 g of navel Chinese herbal medicine was applied each time, two times per day, for a total of 10 consecutive days. Patients from both groups were advised to avoid spicy foods, drink more water, and eat more high-fiber foods. Patients were also asked to maintain a positive emotional state and a healthy lifestyle. The constipation severity of each patient was graded before and after the treatment course. After completion of treatments, the treatment efficacy for each patient was categorized into 1 of 3 tiers:
Recovery: A bowel movement every 2 days. Hard stools becoming softened. No difficulty with bowel movements. No relapse within a short period.
Effective: A bowel movement every 3 days. Hard stools becoming softened. Difficulty with bowel movements improved.
Not effective: No improvement.
The total effective rate for the treatment group was 92.5%, with the following breakdown of improvement tiers: 53 cases fully recovered, 21 cases improvements (effective), 6 cases no improvements. The total effective rate for the treatment group was 78.8% with the following breakdown of improvement tiers: 32 cases fully recovered, 31 cases improvements, 17 cases no improvements. The clinical results of this study demonstrate that post-stroke constipation patients benefit from a combination of electroacupuncture and the Chinese herbal medicine navel paste.
The researchers provide a brief synopsis of the Traditional Chinese Medicine understanding of post-stroke constipation. In Traditional Chinese Medicine, post-stroke constipation is caused by qi deficiency and blood stasis, or yin deficiency and intestinal dryness. Qi deficiency and blood stasis inhibit intestinal peristalsis and therefore lead to constipation. Yin deficiency and intestinal dryness makes stools dry and difficult to move through the intestine.
Tianshu (ST25) is located on the foot Yangming stomach meridian and is a Mu point. Needling Tianshu regulates qi circulation in the intestine and stimulates bowel movements. Fujie and Daheng are located on the foot Taiyin spleen meridian. Tianshu, Fujie, and Daheng are three important acupoints traditionally indicated for the treatment of constipation.
Qihai (CV6) and Guanyuan (CV4) are located on the Ren meridian. Needling these two acupoints tonifies qi and lifts yang. Guilai (ST29) is also named as Changrao (Intestine Winding). In the Zhen Jiu Ji Cheng (Collection of Acupuncture and Moxibustion), it is said that Guilai is indicated for the treatment of constipation. For electroacupuncture, the researchers note that "a disperse-dense wave reinforces the deqi sensation and also activates the intestinal nervous system, which helps to regulate gastrointestinal motility."
The results of the study find acupuncture and topical herbal medicine effective for relieving post-stroke constipation. Although drug therapy is usual care in the majority of hospital settings, the acupuncture and herbal medicine protocol may be an important substitute for drug therapy when drug contraindications are of great concern. The acupuncture and herbal medicine therapy is a treatment option that allows for the reduction of drug intake, thereby simplifying contraindication considerations. Moreover, after a stroke, this is a time of great need for patient, their families, and caregivers. The acupuncture and herbal medicine protocol provides an effective treatment option to assist in the alleviation of suffering.
Reference
Xiong ZH et al. Therapeutic Observation of Abdominal Electroacupuncture plus Chinese Medicinal Application at Umbilicus for Poststroke Constipation [J]. Shanghai Journal of Acupuncture and Moxibustion, 2017, 36(3):265–268.

![Diseases, Symptoms, tcm, [tcmwindow.com]](/uploadFile/adImg/2015/11/11/f5cbfcc0-4df5-4646-9b9a-f316651a0199.jpg)





