Researchers demonstrate that acupuncture is an effective treatment for migraines. The results of their investigation were published in JAMA Internal Medicine (Journal of the American Medical Association). The investigation reveals that acupuncture reduces migraine attack frequency, duration, and intensity. True acupuncture was compared with sham acupuncture and only true acupuncture reduced migraine recurrence rates. Importantly, the effects of true acupuncture provided long-term clinical benefits to migraine sufferers, including lower pain intensity levels and a shorter duration of suffering per each attack.
The researchers find that, "True acupuncture exhibited persistent, superior, and clinically relevant benefits for migraine prophylaxis, reducing the migraine frequency, number of days with migraine, and pain intensity to a greater degree than SA [sham acupuncture] or WL [wait list]." They add that acupuncture produced an additional benefit. Patients receiving true acupuncture demonstrated significant improvements in the "emotional domain of quality of life." The research team concludes, "Acupuncture should be considered as one option for migraine prophylaxis in light of our findings." The title of the work in JAMA Internal Medicine was entitled The long-term effect of acupuncture for migraine prophylaxis: a randomized clinical trial.
The research was a multi-site, randomized clinical trial investigating the efficacy of electroacupuncture for the treatment of chronic migraines. Important factors set this study apart from prior research. Compared with many earlier trials, the team followed subjects over a longer period of time (24 weeks). In addition, the study involved the application of electroacupuncture. Many trials implemented manual acupuncture protocols but there was very little application of electroacupuncture in multi-site, randomized clinical trials prior to this investigation. Notably, this investigation involved the elicitation of the deqi response at all acupuncture points with manual acupuncture followed by the application of electroacupuncture.
The 24-week, randomized study involved 249 subjects (189 women and 69 men). Participants experienced migraines without aura with an attack rate of 2 to 8 times per month. Subjects were divided into three arms. The treatment group received true acupuncture, which was administered at acupoints based on a systematic literature review and a consensus of clinical experts. The second arm was given sham acupuncture at 4 pre-selected non-acupoints. Both groups received electrostimulation. The final wait list group received no treatment for the study duration.
Results
The researchers note that true acupuncture "was more efficacious for migraine prophylaxis than SA [sham acupuncture] or no acupuncture, and the improvement induced by acupuncture persists for at least 24 weeks." The researchers made two additional important discoveries. True acupuncture reduces the pain intensity levels of migraine attacks while simultaneously reducing the overall duration of migraines. The researchers conclude, "Compared with SA [sham acupuncture] and WL [wait list] control groups, TA [true acupuncture] manifested persisting superiority and clinically relevant benefits for at least 24 weeks in migraine prophylaxis, including reducing the number of migraine frequency and days with migraine, as well as decreasing pain intensity."
Prevalence
These findings are important because migraines are debilitating, painful, and widespread. In the USA, millions of people suffer from migraines. Researchers from the Department of Neurology at the Albert Einstein College of Medicine (Bronx, New York) surveyed the USA population and quantified the seriousness of this issue. They conclude, "The number of migraineurs has increased from 23.6 million in 1989 to 27.9 million in 1999 commensurate with the growth of the population. Migraine is an important target for public health interventions because it is highly prevalent and disabling." This staggering statistic indicates that the implementation of acupuncture into mainstream clinical settings may provide important relief for millions of people worldwide.
Design
The semi-protocolized study employed the use of licensed acupuncturists that received a minimum of 5 years of training and 4 years of acupuncture clinical experience. The total number of needles, electroacupuncture settings, and duration of treatment time was identical in the true and sham acupuncture groups; however, sham acupuncture patients did not receive deqi stimulation. For sham acupuncture group patients, a total of 4 non-acupoints were chosen as needle insertion sites. Wait list patients did not receive any treatment but were informed that they would eventually received acupuncture after completion of the study.
True acupuncture patients and sham acupuncture patients received 20 sessions of electroacupuncture treatments at a rate of once per day, for a total of 5 consecutive days. A two day break followed each session prior to applying the next round of sessions. Each acupuncture treatment lasted 30 minutes and the total duration of acupuncture therapy sessions lasted 4 weeks. Participants, all of which were migraineurs without aura, received no form of prophylactic medications for migraines. Ibuprofen (300 mg) was allowed as a rescue medication for severe headaches and was logged into the data.
Acupuncture Points
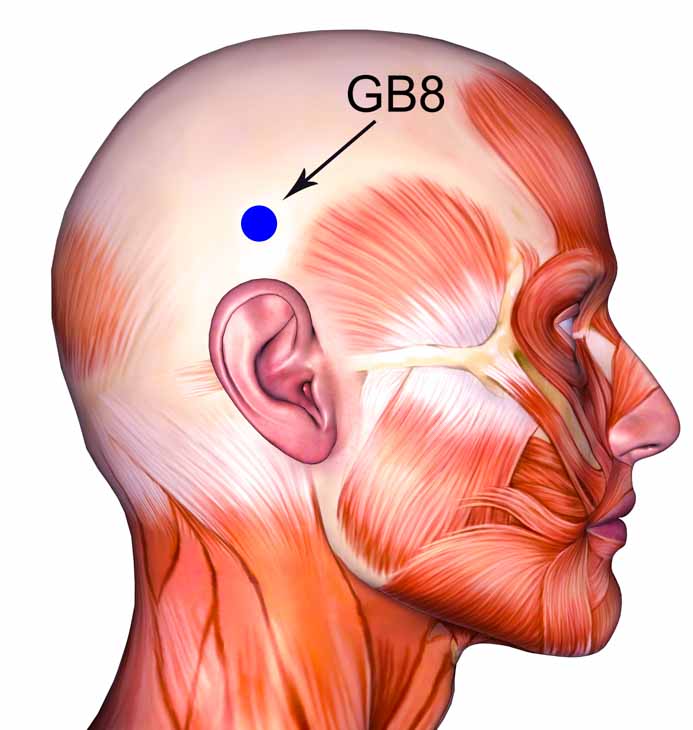
Only 4 acupoints were allowed per acupuncture treatment. Acupuncture point prescriptions were based on a "systematic review of ancient and modern literature," consultation with experts, and prior research. Two primary acupoints were applied to all participants in the true acupuncture group:
Fengchi, GB20 (Wind Pool)
Shuaigu, GB8 (Leading Valley)
An additional 2 acupuncture points were allowed based on syndrome differentiation and headache location based upon presentation along acupuncture meridians. The additional 2 acupoints were limited to a pre-selected set of acupuncture points:
Waiguan, TB5 (Outer Pass)
Yanglingquan, GB34 (Yang Mound Spring)
Kunlun, BL60 (Kunlun Mountains)
Houxi, SI3 (Back Stream)
Hegu, LI4 (Joining Valley)
Neiting, ST44 (Inner Courtyard)
Taichong, LV3 (Great Rushing)
Qiuxu, GB40 (Mound of Ruins)
Only sterile, single-use filiform acupuncture needles were used in the study. This is consistent with modern standards and protocols. Needle length ranged from 25 – 40 mm and all needles had a diameter of 0.25 mm (this is referred to as a 32 Chinese gauge or a 5 Japanese gauge). In an interesting approach to patient care, acupuncture points were applied unilaterally. Left and right side application of acupuncture points were chosen by alternating sides during the needling process. Deqi was stimulated at each acupuncture point. For electroacupuncture, a HANS unit (model LH 200A, Han Institute) was applied with an alternating frequency between 2 and100 Hz. The frequency shifted between each setting every 3 seconds. The intensity was set to patient comfort levels and was limited to 0.1 – 1.0 mA.
Implementation
Acupuncture has been shown to reduce the frequency, duration, and intensity of migraines in a large scale study. The researchers note that migraines affect approximately 14.9% of the population in the USA and approximately 8.4 – 12.7% of the population across Asia. The researchers add that many migraineurs use pharmaceutical medications to ease their suffering; however, this often leads to adverse events including weight gain, fatigue, insomnia, and digestive disturbances. Evidence also indicates that excessive intake of analgesic medications and other medications designed specifically to alleviate migraines may increase the frequency of headaches (Tfelt-Hansen et al.). Given the complexity of controlling migraines and its widespread prevalence, implementation of acupuncture clinics specifically designed to address this condition may improve patient outcomes and alleviate congestion at major medical centers.
References
Zhao, Ling, Jiao Chen, Ying Li, Xin Sun, Xiaorong Chang, Hui Zheng, Biao Gong et al. "The long-term effect of acupuncture for migraine prophylaxis: a randomized clinical trial." JAMA Internal Medicine (2017).
Lipton, Richard B., Walter F. Stewart, Seymour Diamond, Merle L. Diamond, and Michael Reed. "Prevalence and burden of migraine in the United States: data from the American Migraine Study II." Headache: The Journal of Head and Face Pain 41, no. 7 (2001): 646-657. Department of Neurology, Albert Einstein College of Medicine (Bronx, New York).
Tfelt-Hansen PC. Evidence-basedguideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2013;80(9):869-870.
Linde M, Mulleners WM, Chronicle EP, McCrory DC. Valproate (valproic acid or sodium valproate or a combination of the two) for the prophylaxis of episodic migraine in adults. Cochrane Database Syst Rev. 2013;6(6):CD010611.

![Diseases, Symptoms, tcm, [tcmwindow.com]](/uploadFile/adImg/2015/11/11/f5cbfcc0-4df5-4646-9b9a-f316651a0199.jpg)





