TCM Perspective On
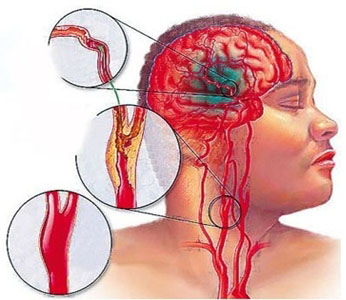
Cerebral Venous ThrombosisCerebral venous thrombosis is also recognized as atherosclerotic and thrombotic cerebral infarction and is caused by the pathological changes of cerebral arterial wall together with elevation of blood coagulation, leading to vascular narrowness, obstruction and ischemic changes of the corresponding cerebral tissue, which may be followed by necrosis. This disease, in traditional
Chinese medicine, is included in the category of "zhong feng" (apoplexy).
Western Point of ViewCerebral venous thrombosis, including thrombosis of cerebral veins and major dural sinuses, is an uncommon disorder in the general population. However, it has a higher frequency among patients younger than 40 years of age, patients with thrombophilia, and women who are pregnant or receiving hormonal contraceptive therapy. Annual incidence is estimated to be 3 to 4 cases per million. The incidence of cerebral venous thrombosis increases to 12 cases per 100 000 deliveries in pregnant women. Cerebral venous thrombosis occurs 3 times as frequently in women, likely because of increased risk during pregnancy and with hormonal contraceptive use.
At least 1 risk factor can be identified in >85% of patients with cerebral venous thrombosis. In the International Study on Cerebral Vein and Dural Sinus Thrombosis cohort, a thrombophilia was noted in 34%, and an inherited thrombophilia was detected in 22%. Inherited thrombophilias associated with cerebral venous thrombosis include deficiencies of antithrombin, protein C, protein S, factor V Leiden mutation, and the prothrombin gene mutation 20210. Antiphospholipid antibodies and hyperhomocysteinemia are acquired prothrombotic states associated with cerebral venous thrombosis.
An additional precipitating factor is often present in patients with thrombophilia who develop cerebral venous thrombosis. Pregnancy, postpartum state, and hormonal contraceptive therapy are the most frequent risk factors in women with cerebral venous thrombosis. Localized infections, such as otitis, mastoiditis, sinusitis, and meningitis and systemic infectious disorders, are also associated with cerebral venous thrombosis. Additional risk factors include chronic inflammatory diseases, such as vasculitides and inflammatory bowel disease, nephrotic syndrome, and malignancy and hematologic disorders, such as polycythemia, essential thrombocytosis, and paroxysmal nocturnal hemoglobinuria. Cerebral venous thrombosis may result from head trauma, local injury to cerebral sinuses or veins, jugular venous cannulation, neurosurgical procedures, and, rarely, lumbar puncture.